Tramadol can cause seizures even at normal doses, especially in people with epilepsy, kidney issues, or those taking certain antidepressants. Learn who’s most at risk and what to do to stay safe.
Tramadol Side Effects: What You Need to Know Before Taking It
When you take tramadol, a synthetic opioid painkiller used for moderate to severe pain. Also known as Ultram, it works by changing how your brain feels pain and can be effective—but it’s not harmless. Many people assume it’s safer than stronger opioids because it’s often prescribed for longer-term use, but that’s a myth. Tramadol carries real risks, and knowing the tramadol side effects could prevent a trip to the ER.
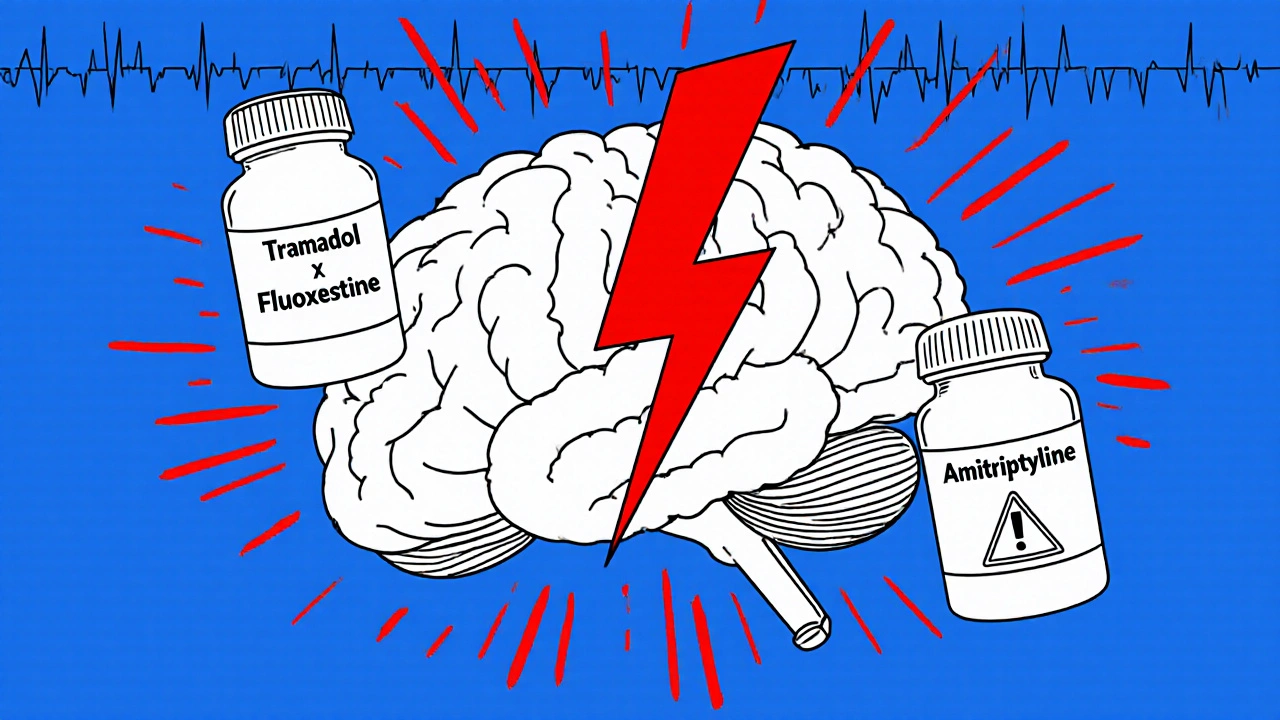
Common side effects include dizziness, nausea, constipation, and headaches. These aren’t rare—they happen to a lot of people, especially when starting the drug. But some reactions are more serious. Trouble breathing, slow heartbeat, or extreme drowsiness can signal an overdose. If you’re taking tramadol with other medicines like antidepressants, anti-anxiety pills, or even some herbal supplements, your risk of dangerous interactions goes up fast. Serotonin syndrome, a rare but life-threatening condition, can happen if tramadol mixes with SSRIs or SNRIs. Your pharmacist should check this every time you refill, but don’t rely on them alone—know your own meds.
Another hidden danger is withdrawal symptoms, the physical and mental reactions that happen when you stop tramadol after using it for more than a few weeks. Also known as opioid withdrawal, it can include anxiety, sweating, shaking, insomnia, and even flu-like symptoms. People often think they can just quit cold turkey, but that’s risky. Tapering off slowly under a doctor’s care makes a huge difference.
And don’t forget about drug interactions, how tramadol behaves when mixed with other substances. It doesn’t just clash with antidepressants—it can also become dangerous with alcohol, muscle relaxers, or even certain cough syrups. Even over-the-counter painkillers like acetaminophen (Tylenol) can add up if you’re taking tramadol in combo products. Always read the labels. If you’re unsure, stop and ask. A quick call to your pharmacy could save your life.
Some users report mood changes, confusion, or even seizures, especially if they have a history of epilepsy or head injuries. Tramadol lowers the seizure threshold, meaning it can trigger seizures even in people who’ve never had one before. It’s not just about pain relief—it’s about balancing risk. If you’re older, have liver or kidney problems, or take multiple meds, your body processes tramadol differently. That’s why personalized care matters.
Below, you’ll find real, practical guides from people who’ve been there—how to track your meds to avoid dangerous combos, how to spot early signs of trouble, and what to do if you think you’ve developed a dependence. These aren’t theoretical tips. They’re from folks who’ve managed tramadol safely—or learned the hard way. You don’t need to guess what’s normal. You can find the answers here.