Tramadol can cause seizures even at normal doses, especially in people with epilepsy, kidney issues, or those taking certain antidepressants. Learn who’s most at risk and what to do to stay safe.
Tramadol and Seizures: What You Need to Know About the Risk
When you take tramadol, a prescription painkiller used for moderate to severe pain that works on both opioid receptors and serotonin/norepinephrine pathways. Also known as Ultram, it’s commonly prescribed because it’s less likely to cause respiratory depression than stronger opioids—but it carries a risk many don’t talk about: seizures, sudden, uncontrolled electrical disturbances in the brain that can cause convulsions, loss of awareness, or muscle spasms.
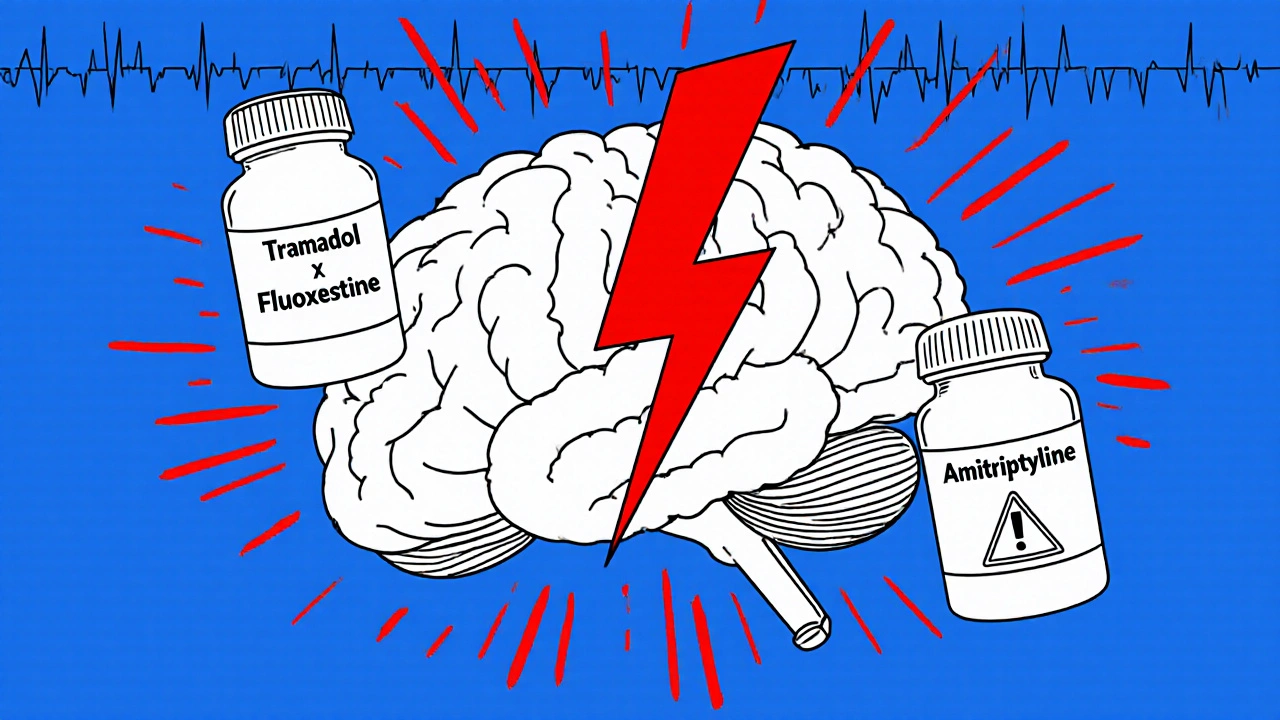
Tramadol lowers the seizure threshold, meaning your brain becomes more easily triggered into a seizure. This isn’t rare—it’s documented in clinical studies and FDA reports. People taking high doses, those with a history of epilepsy, head injuries, or alcohol withdrawal, or those mixing tramadol with antidepressants like SSRIs or SNRIs are at higher risk. Even someone who’s never had a seizure before can be affected if they’re on the wrong combo of meds. The risk jumps sharply above 400 mg per day, but it can happen at lower doses too, especially if you’re sensitive or have liver or kidney issues.
It’s not just about the dose. drug interactions, when two or more medications affect each other’s behavior in the body play a big role. For example, combining tramadol with Wellbutrin, Prozac, or even some over-the-counter cough syrups can spike serotonin levels and push your brain past its limit. That’s why checking your full medication list with your pharmacist isn’t just smart—it’s lifesaving. You might think you’re managing pain safely, but if you’re also taking something for anxiety, depression, or even a cold, you could be quietly increasing your seizure risk.
Signs aren’t always dramatic. A sudden stiffening of limbs, staring blankly for a few seconds, or a strange taste in your mouth before a headache could be a warning. If you’ve ever felt like your body "short-circuited" for a moment, even once, tell your doctor. Don’t wait for a full-blown seizure. Stopping tramadol cold turkey can also trigger seizures, so if you need to quit, do it slowly under medical supervision.
Below, you’ll find real, practical guides from people who’ve navigated this exact issue—how to track your meds to avoid dangerous combos, how to spot hidden risks in common pain relievers, and what to do if you’re already on multiple medications. These aren’t theoretical tips. They’re from folks who’ve been there, checked their lists, talked to their pharmacists, and made changes that kept them safe.