Tramadol can cause seizures even at normal doses, especially in people with epilepsy, kidney issues, or those taking certain antidepressants. Learn who’s most at risk and what to do to stay safe.
Opioid Seizure Risk: What You Need to Know About Safety and Prevention
When you take opioids, a class of pain-relieving drugs that include oxycodone, hydrocodone, morphine, and fentanyl. Also known as narcotics, they work by binding to brain receptors to reduce pain—but they also affect electrical activity in the brain, which can trigger seizures in some people. This isn’t rare. Studies show that even at prescribed doses, certain opioids like methadone and tramadol carry a higher risk of seizures, especially if you have other health issues or take them with other meds.
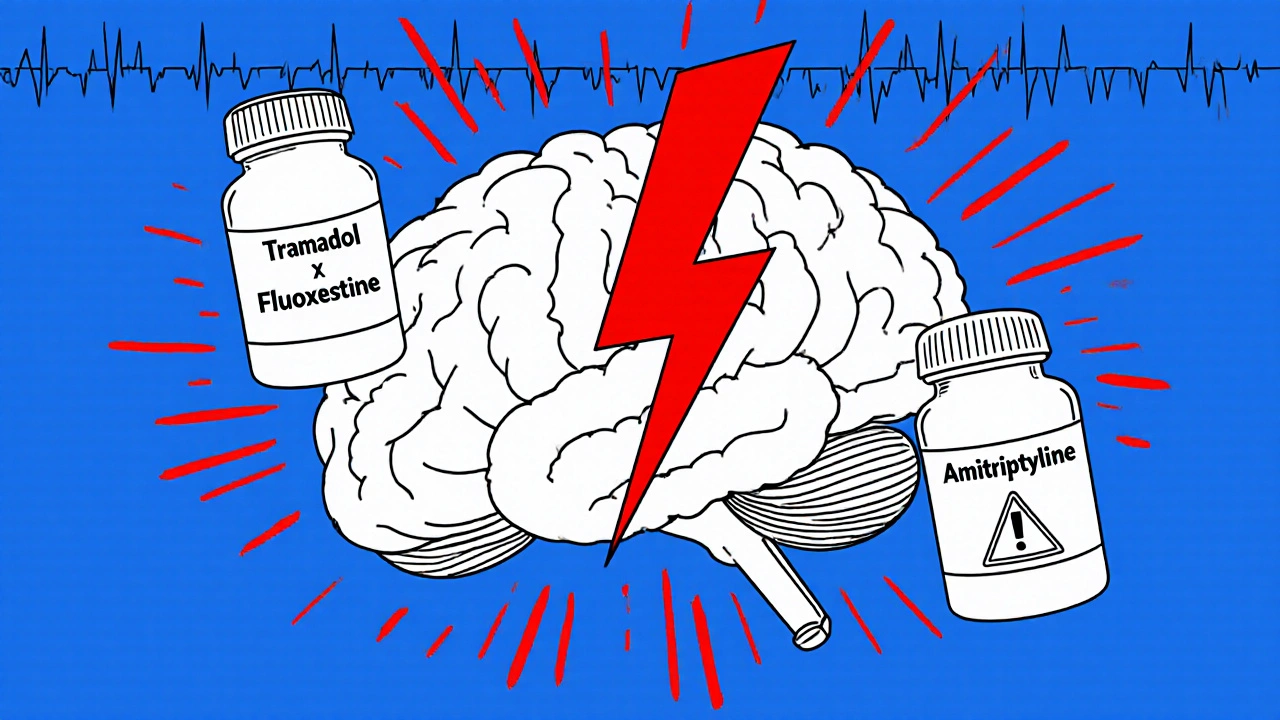
The seizure risk, a sudden, uncontrolled electrical disturbance in the brain that can cause convulsions, loss of awareness, or muscle spasms doesn’t just happen with overdose. It can occur in people taking opioids exactly as directed. Factors like kidney or liver problems, older age, a history of epilepsy, or mixing opioids with antidepressants, stimulants, or even some antibiotics can raise the chance. Even something as simple as suddenly changing your dose—skipping a day or doubling up—can tip the balance. medication interactions, when two or more drugs affect each other’s effects in the body are a major hidden danger. Many people don’t realize that common OTC painkillers or sleep aids can interact with opioids in ways that lower the seizure threshold.
It’s not about avoiding opioids altogether—it’s about knowing your personal risk. If you’ve been on opioids for chronic pain, ask your pharmacist: "Could this medicine trigger seizures for me?" Check your list of all medications, including supplements. A personal medication list, a written or digital record of all drugs, doses, and allergies you take isn’t just for emergencies—it’s your first line of defense. Tools like the FDA or WebMD interaction checkers can help, but they’re not perfect. That’s why talking to a real person—your pharmacist—is still the best protection.
Some people mistake seizure symptoms for side effects like dizziness or nausea. If you feel a strange tingling, sudden confusion, or unexplained muscle jerks, don’t brush it off. These could be early signs. Keeping your dose stable, avoiding alcohol, and staying hydrated can help reduce risk. And if you’re on methadone or tramadol, your doctor should monitor you more closely—especially if you’re over 65 or have a history of head injury.
Below, you’ll find real, practical guides from people who’ve been there. Whether you’re managing chronic pain, helping a loved one, or just trying to avoid dangerous mix-ups, these posts give you the clear, no-fluff facts you need to stay safe. No theory. No guesswork. Just what works.