BPH-Back Pain Symptom Checker
This tool helps you assess whether your back pain might be related to an enlarged prostate (BPH). Answer the following questions about your symptoms:
Your Results:
Ever felt a nagging ache in your lower back and wondered if it’s just a sore muscle or something deeper? For many men over 50, that ache might be linked to an enlarged prostate. This article breaks down why benign prostatic hyperplasia (BPH) can cause lower back pain, how to spot the connection, and what practical steps you can take to feel better.
What Is Benign Prostatic Hyperplasia?
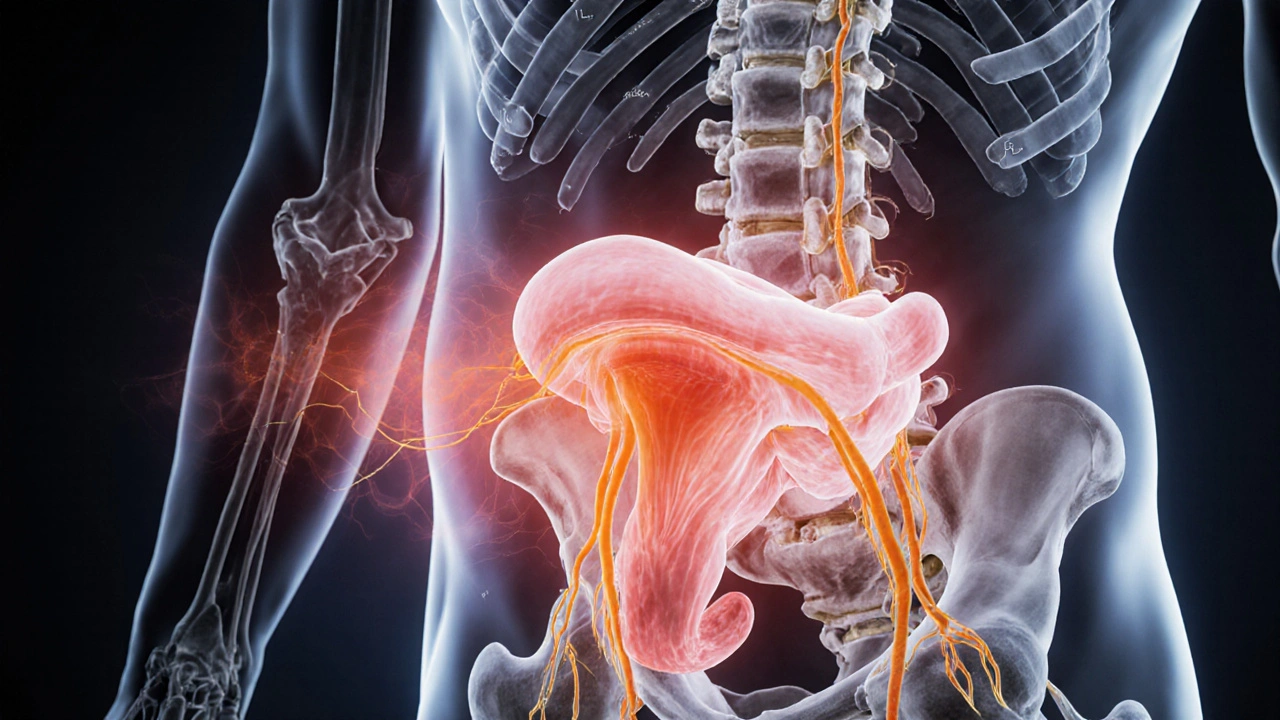
Benign prostatic hyperplasia is a non‑cancerous enlargement of the prostate gland that occurs as men age. The prostate sits just below the bladder and surrounds the urethra, so when it grows it can press on the urinary tract, leading to symptoms like frequent urination, weak stream, and nighttime trips to the bathroom. First described in the early 1900s, BPH now affects roughly 50% of men over 60 and up to 70% of men in their 70s.
Understanding Lower Back Pain
Lower back pain is a broad term that covers any discomfort from the lumbar spine to the sacrum. Causes range from muscle strain and disc degeneration to nerve irritation and referred pain from nearby organs. Because the spine shares nerve pathways with the pelvic region, pain originating in the prostate can travel up the lower back, masquerading as a simple “backache.”
Why BPH Can Lead to Back Pain
The link isn’t magic; it’s anatomy and physiology working together. Here are the main ways an enlarged prostate can make your back hurt:
- Nerve compression: The prostate lies close to the pudendal and sacral nerves that also supply the lower back. As the gland swells, it can press on these nerves, sending pain signals upward.
- Pelvic floor tension: BPH often causes urinary urgency and incomplete emptying. The pelvic floor muscles respond by tightening, and chronic tension radiates to the lumbar region.
- Inflammation spill‑over: Chronic prostatitis‑like inflammation can release cytokines that irritate nearby tissues, including the fascia surrounding the spine.
- Hormonal shifts: Elevated dihydrotestosterone (DHT) that drives prostate growth also affects muscle tone and may contribute to spinal discomfort.
- Postural changes: Men with BPH may adopt a forward‑leaning stance while urinating or sitting for long periods, straining the lumbar spine over time.
Who’s Most at Risk?
If you’re over 50, have a family history of prostate issues, lead a sedentary lifestyle, or carry extra weight around the abdomen, you’re higher on the risk ladder. Diabetes, high blood pressure, and smoking also increase the likelihood of both BPH and back‑related problems.
Spotting the Overlap: Signs That Your Back Pain Might Be BPH‑Related
Not every ache points to the prostate, but look out for these clues:
- Back pain worsens after a full bladder or during a night‑time bathroom trip.
- You notice a dull, deep ache rather than a sharp, localized strain.
- Urinary symptoms (frequency, urgency, weak stream) appear alongside the back discomfort.
- Physical therapy for the back offers limited relief until urinary issues are addressed.
If two or more of these patterns show up, it’s worth discussing the connection with a GP or urologist.
How Doctors Diagnose the Connection
The evaluation is usually a two‑part process:
- Prostate assessment: Digital rectal exam (DRE), prostate‑specific antigen (PSA) test, and possibly an ultrasound to gauge size.
- Back assessment: Physical exam, range‑of‑motion tests, and imaging (X‑ray or MRI) to rule out structural spine issues.
When both sets of findings point to an enlarged prostate and no major spinal pathology, clinicians often label the back discomfort as “referred pain from BPH.”

Managing the Dual Issue: Treatment Options That Hit Both Targets
Here’s where things get practical. Treating the prostate can alleviate the back pain, and vice‑versa. Below is a quick look at common BPH therapies and their side‑effects on the lower back.
| Medication | Mechanism | Effect on Urinary Symptoms | Potential Back‑Pain Influence | Common Side Effects |
|---|---|---|---|---|
| Alpha‑blockers (e.g., tamsulosin) | Relax smooth muscle in prostate and bladder neck | Quick relief of flow issues | May reduce pelvic floor tension, easing back ache | Dizziness, ejaculatory issues |
| 5‑Alpha‑Reductase Inhibitors (e.g., finasteride) | Block DHT, shrinking prostate over months | Long‑term reduction in gland size | Gradual decrease in nerve compression → less back pain | Sexual dysfunction, decreased libido |
| Phytotherapy (saw‑palmetto, beta‑sitosterol) | Anti‑inflammatory, mild DHT inhibition | Modest symptom relief | Some men report reduced pelvic discomfort | GI upset, rare allergic reactions |
| Physical therapy & core strengthening | Improves posture, relieves pelvic floor strain | Supports urinary function | Directly targets lumbar muscles, reduces pain | Minimal |
Beyond meds, consider these integrated strategies:
- Pelvic floor physiotherapy: Teaches relaxation techniques that lower pressure on the prostate and back.
- Regular aerobic activity: Walking, swimming, or cycling improves circulation, reduces inflammation, and supports weight control.
- Heat therapy: Warm sits or lumbar heat packs can soothe muscle tension caused by pelvic floor over‑use.
- Diet tweaks: Reduce caffeine and alcohol, increase omega‑3 rich foods (salmon, flaxseed) to lessen inflammation.
Prevention Tips: Keeping Both Prostate and Spine Happy
Staying ahead of the problem is easier than fixing it later. Here are five habit changes that protect both organs:
- Maintain a healthy waistline - abdominal fat squeezes the pelvis and adds pressure on the lumbar spine.
- Stay hydrated but time fluid intake: drink plenty during the day, cut back 2‑3hours before bedtime to reduce night‑time bladder spikes.
- Practice gentle stretching for the hips, hamstrings, and lower back daily; tight hips can pull on the pelvic floor.
- Schedule regular check‑ups after age50; early detection of prostate growth can prevent chronic back strain.
- Quit smoking - it worsens both vascular supply to the prostate and disc health.
Quick Self‑Assessment Checklist
- Do you experience frequent nighttime urination (≥2times)?
- Is your lower back ache more noticeable after a full bladder?
- Have you noticed a weak or interrupted urine stream?
- Does pelvic floor tightening or constipation accompany the pain?
If you answered “yes” to three or more, book a visit with your GP and mention the possible BPH‑back pain link.
Frequently Asked Questions
Can back pain be the first sign of BPH?
Yes. In many men, especially those over 60, the first noticeable symptom is a dull ache in the lower back that worsens after urination. It’s often missed because people assume it’s a simple muscle strain.
Do alpha‑blockers actually relieve back pain?
Alpha‑blockers relax the smooth muscle at the bladder neck and prostate, which can reduce pelvic floor tension. Many patients report a noticeable drop in back discomfort within weeks of starting the medication.
Should I get an MRI if I have back pain and BPH?
An MRI is useful if you have red‑flag symptoms like numbness, weakness, or severe localized pain. For routine BPH‑related aches, a thorough physical exam and prostate assessment are usually enough.
Can lifestyle changes shrink the prostate?
While diet and exercise don’t reverse large‑scale growth, they can slow progression. Weight loss, reduced alcohol, and regular cardio have been shown to lower PSA levels and alleviate both urinary and back symptoms.
Is surgery ever needed for back pain caused by BPH?
Surgery is rare for pain alone. It’s considered when the prostate is very large, causing severe urinary obstruction and persistent nerve compression that haven’t responded to meds or physiotherapy.

15 Comments
Daisy canales
October 7 2025
Yeah sure the prostate’s the secret mastermind behind every back ache.
keyul prajapati
October 8 2025
It is indeed fascinating how an organ that most men only think about when they are in the bathroom can have such a widespread influence on the musculoskeletal system. The anatomy of the pelvic floor creates a network of nerves that do not respect the artificial boundaries we draw between urinary and spinal health. When the prostate enlarges, it can exert pressure on the pudendal nerve, a conduit that also sends sensations up toward the lumbar region. Moreover, chronic urinary urgency often forces men to adopt a guarded posture, which in turn places additional load on the lower back muscles. Over time, this postural adaptation can evolve into a persistent ache that is mistakenly attributed to a simple strain. Inflammation associated with BPH, sometimes resembling chronic prostatitis, releases cytokines that can sensitize nearby tissues, including the fascia surrounding the vertebrae. Hormonal shifts, particularly increased dihydrotestosterone, are known to affect not only prostate size but also muscle tone, potentially contributing to spinal discomfort. Lifestyle factors such as sedentary behavior and abdominal obesity further exacerbate the mechanical stresses on both the prostate and the lumbar spine. The interplay between these factors creates a feedback loop where urinary symptoms worsen back pain, and the resulting discomfort encourages behaviors that aggravate the prostate. Clinical observations support this bidirectional relationship, as patients often report relief from back pain after successful medical management of BPH. Therefore, recognizing the prostate as a possible source of lower back pain is essential for comprehensive patient care. Screening tools that incorporate both urinary and spinal symptoms can aid in early identification of this overlap. Treatment strategies that combine alpha‑blockers with pelvic floor physiotherapy have shown promising results in breaking the cycle. Ultimately, a multidisciplinary approach that considers the interconnectedness of the urinary and musculoskeletal systems offers the best chance for lasting relief.
Alice L
October 9 2025
Dear readers, I wish to convey, with the utmost respect and decorum, that the elucidation provided herein regarding the correlation between benign prostatic hyperplasia and lumbar discomfort is both thorough and commendable. The author has adeptly navigated complex anatomical concepts, presenting them in a manner befitting an academic symposium. One must applaud the inclusion of comprehensive preventative measures, which reflect a holistic view of men's health. Moreover, the systematic presentation of diagnostic pathways demonstrates a rigorous clinical mindset. In sum, the discourse stands as an exemplary model of patient‑centered education.
Seth Angel Chi
October 10 2025
While the article is thorough it overlooks the fact that most men never need medication for minor aches the market pushes unnecessary drugs
Kristen Ariies
October 11 2025
Wow! This is exactly the kind of boost we need to take charge of our health! 🎉 Understanding that a swollen prostate can be the hidden culprit behind that nagging back pain is a game‑changer. Let’s not wait for the pain to dictate our lives-let’s act now! Start with a simple daily stretch routine, stay hydrated, and consider a gentle pelvic floor exercise. Remember, consistent aerobic activity like walking or swimming can do wonders for both the prostate and the spine. Keep the momentum going and share these insights with the guys who might be suffering in silence-together we can make a real difference! 💪
Ira Bliss
October 12 2025
Thanks for the thorough breakdown! 🙌 I’ve been dealing with nighttime trips and a dull back ache for months, and this really puts things into perspective. I’m going to schedule a check‑up and maybe try a short pelvic floor routine first. Also, any tips on diet tweaks? I’ve heard omega‑3 helps, but would love some concrete suggestions! 😃
Donny Bryant
October 13 2025
Good info. I’m a guy over 50 and I’ve had the same symptoms. Going to see my doctor soon.
kuldeep jangra
October 14 2025
First of all, thank you for shedding light on a topic that many men tend to ignore until it becomes unbearable. I have personally experienced the confusing mix of frequent nighttime trips and that stubborn lower back ache that seems to linger after a full bladder. The way you described the nerve compression and pelvic floor tension made me realize why my usual back stretches weren’t helping. Incorporating pelvic floor physiotherapy, as you suggested, will be my next step, alongside the core strengthening exercises you listed. Additionally, I plan to adjust my fluid intake schedule-drinking more during daylight hours and cutting back in the evening-to see if that reduces the nightly urgency. Your dietary recommendations are also spot on; I’ll start adding more omega‑3 rich foods like salmon and maybe even a flaxseed supplement. Finally, I appreciate the emphasis on regular check‑ups after age 50; I’ll be sure to book an appointment with my urologist soon. Thank you for such a comprehensive guide-it’s truly empowering to have actionable steps to improve both prostate health and back comfort.
harry wheeler
October 15 2025
Interesting read I think many men overlook the prostate back pain link and focus only on the spine
faith long
October 16 2025
Enough with the polite talk – this is serious! Men are letting their backs suffer because they’re too embarrassed to talk about a busted prostate. Stop ignoring the signs and get a real doctor, not some online chatbot, to check that swollen gland. The article mentions meds but many of those have nasty side effects that aren’t mentioned properly. Push for a proper evaluation and don’t settle for “just stretch your back”. It’s time to demand comprehensive treatment that addresses both the prostate and the spine, or you’ll keep living with that pain forever.
Danny Wakefield
October 17 2025
Alright folks, strap in because the real story is way deeper than a simple prostate‑back pain link. The pharmaceutical giants are feeding us pills to mask symptoms while they keep the research money flowing. Have you ever noticed how every new drug comes with a new set of side effects? It’s a classic push‑pull strategy to keep you dependent. I’m not saying ignore all meds, but you need to question why we’re not seeing more natural, holistic approaches being promoted. Also, the whole “sit properly while urinating” thing is just a distraction from the bigger issue of our lifestyle choices being engineered by the system. Stay vigilant, share this info, and keep your eyes open. The truth is out there!
Samantha Dean
October 18 2025
In contemplating the interrelation of prostatic enlargement and lumbar discomfort, one must acknowledge the inherent unity of the corporeal whole. The body, as Aristotle posits, operates as an integrated system wherein perturbations in one region reverberate through others. Thus, a nuanced appreciation of anatomical and physiological convergence is requisite for a comprehensive therapeutic approach. By embracing this philosophical lens, we transcend reductionist treatments and foster a more holistic praxis.
Vanessa Peters
October 19 2025
Wow, this article really hits the nail on the head! The drama of a sneaky prostate causing back pain is like a plot twist you never saw coming. Kudos to the author for exposing the hidden villain in our bodies!
Suzan Graafstra
October 20 2025
Ah, the prostate-nature's enigmatic sphincter of mystery-whispers to the spine with a subtle yet relentless sigh. In the theater of the human form, such a silent playwright may very well dictate the cadence of our aches. Let us, therefore, honor this hidden maestro, lest we ignore the quiet symphonies that echo within our own flesh.
Kripa Mohamed
October 21 2025
Cool info. I’ll try some stretches and see a doc.